In a truly extraordinary feat of medical intervention aimed at preserving life, surgeons successfully sustained a gravely ill gentleman for a two-day period without any native lungs. This critical timeframe allowed him to await a bilateral lung transplant, a pioneering strategy that may potentially be revisited for carefully selected individuals.
A dedicated contingent from Northwestern University in the United States engineered a comprehensive artificial lung (TAL) apparatus. This system diligently oxygenates circulating blood, mimicking the vital function of natural lungs, while simultaneously managing hemodynamics and safeguarding cardiac integrity.
The TAL proved instrumental in stabilizing the patient’s condition, thereby preparing him for the intricate procedure of receiving donor lungs. Over two years subsequent to the operation, the individual has achieved a substantial recovery, boasting fully functional pulmonary organs.
This remarkable narrative originates in the spring of 2023, when the 33-year-old patient succumbed to influenza-induced respiratory failure. This condition rapidly deteriorated into sepsis and pneumonia, culminating in a severe presentation of acute respiratory distress syndrome (ARDS).
“He had contracted a pulmonary infection so virulent that it proved resistant to all antibiotic treatments,” explains thoracic surgeon Ankit Bharat.
“This virulent infection led to the liquefaction of his lungs and subsequently disseminated throughout his entire system.”
The conventional medical response would typically involve placing the patient on life support equipment, affording the damaged lungs an opportunity to recuperate. However, in this specific instance, the lungs themselves were the primary source of the affliction and the infectious process. The patient’s prognosis appeared dire, with a high likelihood of mortality whether his lungs were excised or retained.
The surgical removal of both lungs, a procedure known as bilateral pneumonectomy, frequently precipitates cardiac decompensation due to significant alterations in blood flow dynamics.
To circumvent this perilous outcome and surmount the inherent constraints encountered in prior experimental endeavors, the medical team responsible for the TAL integrated dual blood flow conduits and a flow-adaptive shunt. This sophisticated configuration effectively mitigates fluctuations in circulatory flow.
The artificial apparatus proved sufficiently robust to maintain the patient’s vital functions, allowing his physique to stabilize sufficiently for a lung transplant to become a feasible option. Following the excision of the compromised organs, initial indicators of infection resolution began to emerge.
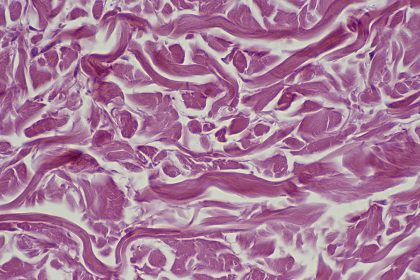
Bharat and his colleagues conducted a meticulous molecular examination of the excised lungs, confirming the irreversible nature of the damage and the absence of any possibility for spontaneous recovery from ARDS.
The extensive fibrotic scarring and immunological damage rendered a lung transplant an absolute necessity in this particular clinical scenario.
“Typically, lung transplantation is reserved for individuals with chronic pulmonary ailments such as interstitial lung disease or cystic fibrosis,” observes Bharat.
“Currently, the prevailing belief is that in cases of severe ARDS, continuous supportive care will ultimately lead to pulmonary recovery.”
This innovative approach holds the potential to be replicated, thereby saving additional lives. Although the construction of a TAL system of this complexity is presently feasible only within highly specialized medical institutions, Bharat expresses optimism that the advancements implemented in this case could be integrated into conventional medical devices in the future.
Whereas a lung transplant might have been deemed an improbable intervention in such circumstances previously, it has now been demonstrably proven to be achievable and successful, potentially becoming a viable option for future patients, contingent upon the timely availability of donor organs.
“In my clinical experience, young patients succumb with alarming regularity due to a lack of awareness that transplantation is a viable therapeutic avenue,” states Bharat.
“For critical pulmonary damage stemming from respiratory infections, even in acute settings, a lung transplant can be a life-saving intervention.”
A detailed account of this operative procedure has been formally documented and published in the esteemed journal Med.