An extensive examination of health documentation spanning five years, encompassing over 130,000 adults diagnosed with insomnia who had been utilizing melatonin for a minimum of twelve months, revealed a heightened propensity for heart failure diagnoses, subsequent hospitalizations due to this cardiac condition, or mortality from any cause.
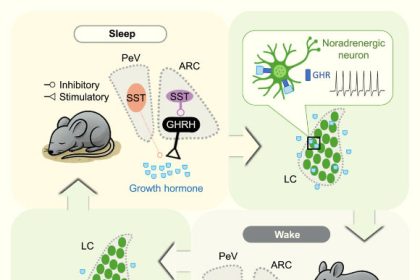
Melatonin is a naturally occurring hormone secreted by the pineal gland, instrumental in regulating the human body’s circadian rhythms, specifically the diurnal cycle of wakefulness and sleep.
The synthesis and release of melatonin are amplified during periods of darkness and diminish in the presence of daylight.
Synthetic compounds, chemically identical to the endogenous hormone, are frequently employed therapeutically for the management of insomnia (characterized by difficulties initiating or maintaining sleep) and the mitigation of jet lag symptoms.
These supplemental preparations are readily accessible without a prescription in numerous global markets, including the United States.
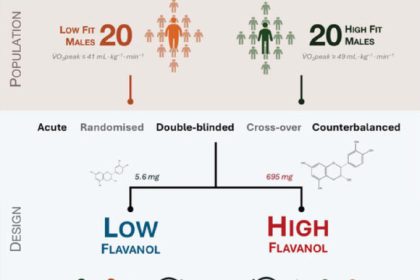
Within the scope of a recent investigative undertaking, participants were categorized based on their history of sustained melatonin ingestion, with “long-term use” meticulously defined as a period of one year or more, as evidenced by their electronic health records, thus forming the “melatonin cohort.”
Conversely, individuals whose medical histories contained no mention of melatonin usage were designated as belonging to the “non-melatonin cohort.”
“The assumption that melatonin supplements are entirely benign may warrant reevaluation,” posited Dr. Ekenedilichukwu Nnadi, affiliated with SUNY Downstate/Kings County Primary Care.
“Should our findings be corroborated, this could significantly influence the counsel healthcare providers offer patients regarding sleep-enhancing agents.”
As per the American Heart Association’s 2025 Statistical Report on Heart Disease and Stroke, heart failure transpires when the cardiac muscle’s pumping efficiency is compromised, failing to adequately perfuse the body’s organs with oxygenated blood essential for their proper functioning. This condition represents a prevalent health concern, impacting an estimated 6.7 million adults in the United States.
Leveraging an extensive international repository of health data, the research team meticulously analyzed five years of electronic health records for adult individuals diagnosed with chronic insomnia who had documented melatonin use exceeding one year.
These individuals were carefully matched with comparable subjects from the database who also suffered from insomnia but had no record of melatonin consumption.
Participants who had a pre-existing diagnosis of heart failure or had been prescribed alternative pharmacological interventions for sleep disorders were systematically excluded from the analytical process.
The scientific inquiry revealed that among the studied adult population with insomnia, those whose electronic health records indicated prolonged melatonin use (a minimum of 12 months) exhibited an approximately 90% elevated probability of developing incident heart failure over the five-year observation period, in comparison to their matched counterparts who did not use melatonin (4.6% versus 2.7%, respectively).
A comparable elevated risk was observed (82% higher) when the researchers focused on individuals who had at least two melatonin prescriptions filled with a minimum interval of 90 days between them.
In a subsequent secondary analysis, the investigators determined that participants who were prescribed melatonin were nearly 3.5 times more likely to be admitted to a hospital for treatment of heart failure when contrasted with those who were not utilizing melatonin (19.0% versus 6.6%, respectively).
Furthermore, individuals within the melatonin-consuming cohort demonstrated a nearly twofold higher likelihood of succumbing to mortality from any cause when compared to the non-melatonin group (7.8% versus 4.3%, respectively) over the aforementioned 5-year interval.
“Melatonin supplements are widely perceived as a safe and ‘natural’ recourse for promoting improved sleep, thus it was striking to observe such consistent and statistically significant escalations in adverse health outcomes, even subsequent to statistical adjustments for numerous confounding risk factors,” Dr. Nnadi remarked.
“I find it surprising that physicians would endorse melatonin for insomnia and advise patients on its use beyond 365 days, particularly since, in the U.S. context, melatonin is not formally indicated for the therapeutic management of insomnia,” commented Dr. Marie-Pierre St-Onge from Columbia University.
“Within the United States, melatonin is available as an over-the-counter dietary supplement, and it is imperative that individuals recognize it should not be consumed on a chronic basis without a clearly established medical indication.”
The complete findings of this study are scheduled for presentation at the 2025 Scientific Sessions of the American Heart Association, occurring concurrently this week.