While the emergence of cancer might be an unavoidable consequence of cellular replication and, by extension, existence itself, the United States has witnessed substantial advancements in its battle against this formidable affliction. A notable achievement is the attainment of a quinquennial survival rate exceeding 70 percent for individuals diagnosed with cancer between 2015 and 2021.
The most pronounced improvements in survival outcomes have been observed in cases involving advanced or terminal stages of the disease.
Enhanced early detection capabilities, refined screening methodologies, superior treatment modalities, and a decline in smoking participation have contributed to the averting of an estimated 4.8 million cancer-related fatalities in the US from 1991 to 2023. This translates to an additional 3,256,800 men and 1,555,300 women being granted an extended lifespan.
These critical findings, meticulously compiled by researchers affiliated with the American Cancer Society (ACS), were recently brought to light in the publication titled Cancer Statistics 2026.
“Presently, seven out of every ten individuals can expect to survive their cancer diagnosis for five years or longer, a significant increase from only half of patients in the mid-1970s,” commented Rebecca Siegel, a cancer epidemiologist and the principal author of the study, in a recent statement.
“This remarkable triumph is predominantly attributable to decades of dedicated cancer research, which has equipped clinicians with potent tools to combat the disease more effectively, thereby transforming numerous cancer diagnoses from a terminal prognosis into a manageable chronic condition.”
The 2026 report signifies the 75th consecutive year the ACS has been instrumental in disseminating vital cancer survival statistics, aiming to bolster public comprehension and elevate public health initiatives.
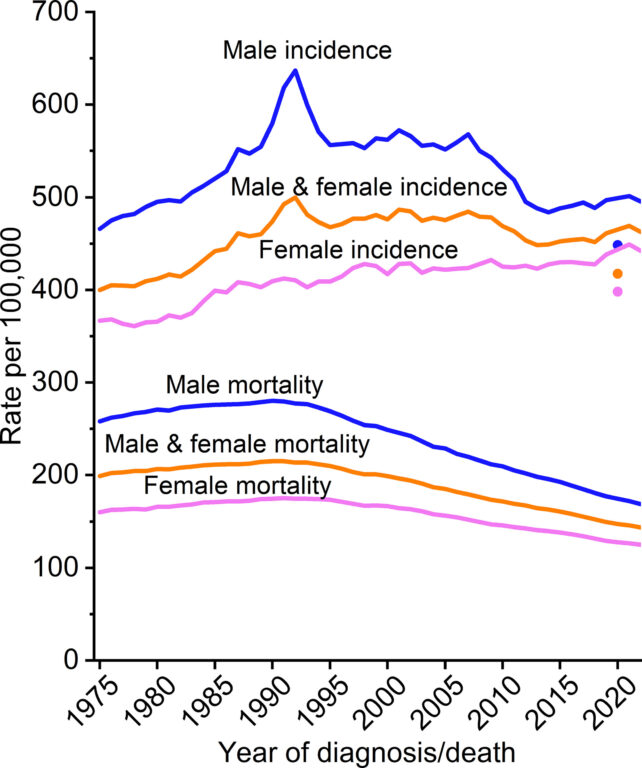
The document encapsulates the most current, population-wide incidence and mortality data, reflecting rates up to 2022 and 2023, respectively. It is important to note that this data inherently lags behind the current calendar year due to the exhaustive process involved in data acquisition, collation, validation, and dissemination.
Cancer stands as the second leading cause of mortality in the US, surpassed only by cardiovascular disease. However, the overall quinquennial survival rates have now reached unprecedented highs, escalating from 49 percent for diagnoses during the 1970s to an impressive 70 percent for diagnoses recorded between 2015 and 2021.
Moreover, the most substantial advancements in survival rates were noted for cancers that had metastasized to other bodily regions, with survival rates more than doubling from a mere 17 percent in the mid-1990s to 35 percent during the 2015-2021 period.
Survival outcomes exhibited considerable variability across different cancer typologies.
“Current survival rates are exceptionally high for cancers affecting the thyroid (98 percent), prostate (98 percent), testes (95 percent), and melanoma (95 percent). Conversely, survival is notably lower for cancers of the lung (28 percent), liver (22 percent), esophagus (22 percent), and pancreas (13 percent),” as detailed by the researchers in their report.
Disparities in incidence and mortality rates were also evident, influenced by factors such as socioeconomic standing, race, and ethnic background. Indigenous populations in North America demonstrated the highest rates of cancer mortality. For illustration, their mortality rates for cancers of the kidney, liver, stomach, and uterine cervix are approximately twice those observed in the White population.
Furthermore, geographical variations in cancer outcomes were intrinsically linked to state and local health policies, as well as the accessibility and affordability of health insurance. Consequently, cancer mortality rates fluctuated between 122 to 128 deaths per 100,000 individuals in states like Utah, Hawaii, New York, and Colorado, contrasting with rates of 178 to 180 deaths per 100,000 in states such as West Virginia, Mississippi, and Kentucky.
Preventative practice adoption also showed divergence, with human papillomavirus (HPV) vaccination coverage rates for adolescents aged 13-17 ranging from a low of 38 percent in Mississippi to a high of 84 percent in Rhode Island.
On a national scale, pediatric cancer mortality has experienced a reduction exceeding two-thirds, decreasing from six fatalities per 100,000 in 1970 to two per 100,000 in 2023.
Adolescent mortality rates have likewise seen a significant decline over the same timeframe, falling from seven per 100,000 to three per 100,000. A substantial contributor to this reduction is the notable improvement in leukemia survival rates, achieved through the optimization of treatment regimens.
Temporal dynamics also play a crucial role. Medical professionals may soon anticipate an increase in advanced cancer diagnoses due to the disruption in early detection efforts caused by the COVID-19 pandemic. For instance, the curtailment of colorectal cancer screening during the pandemic could result in as many as 7,000 excess deaths by the year 2040. However, a recent resurgence in screening activities, particularly driven by increased utilization of stool-based tests, may serve to mitigate this projected mortality increase.
The report includes projections for future cancer incidence and mortality. It is anticipated that in 2026, the United States will witness over 2,100,000 new cancer diagnoses (averaging approximately 5,800 cases daily) and nearly 630,000 deaths (averaging around 1,720 fatalities daily).
Lung cancer is projected to be the leading cause of cancer-related mortality, accounting for more deaths than colorectal cancer (the second highest) and pancreatic cancer (the third highest) combined.
In conclusion, despite the encouraging upward trajectory of survival rates, sustained progress remains susceptible to numerous challenges. These include the escalating incidence rates observed for prevalent cancers such as breast, prostate, and pancreatic cancers.
“Potential reductions in funding for cancer research and significant impacts on access to health insurance coverage could potentially reverse these hard-won gains and impede future scientific breakthroughs,” stated Shane Jacobson, CEO of the ACS, in a recent address.
“We cannot afford to cease our efforts at this juncture. A considerable volume of work still lies ahead.”
This comprehensive research has been formally published in the esteemed journal CA: A Cancer Journal for Clinicians.







