Emerging research originating from Japan has once again illuminated the profound connection between oral well-being and cognitive vitality; a link widely acknowledged by the medical fraternity as surprisingly significant.
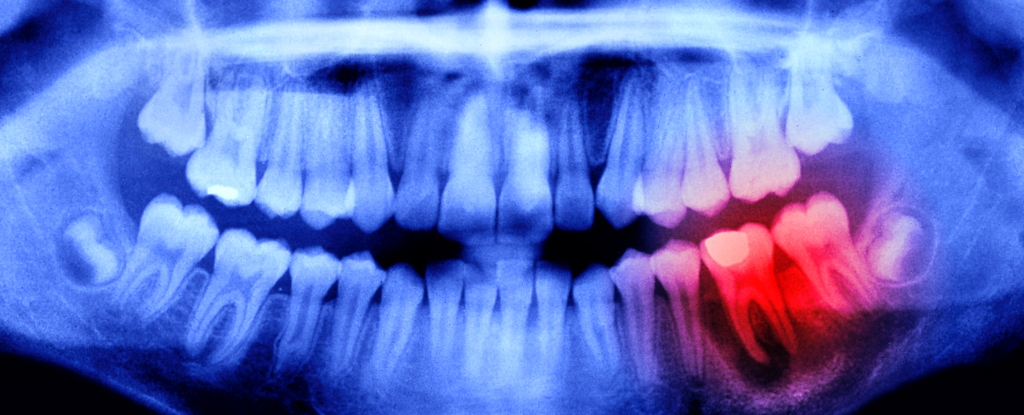
This investigation sought to ascertain whether oral afflictions such as periodontitis (gum disease) and the loss of dentition could elevate the susceptibility to neurodegenerative conditions, including cerebrovascular accidents (strokes), Alzheimer’s disease, and various other forms of cognitive impairment.
The findings were unequivocal: both aforementioned oral health issues are correlated with an accelerated rate of hippocampal atrophy. The hippocampus, a critical brain structure, is instrumental in governing memory retention, learning processes, and emotional regulation. While this represents a consequential discovery, it is by no means the inaugural instance of such a correlation being established.
In March, a comprehensive US study involving over 40,000 participants enlisted in the UK Biobank research initiative concluded that suboptimal oral hygiene appears to constitute a principal risk determinant for both stroke and dementia.
Further reinforcing this notion, a 2019 review of existing literature by another research collective posited that “collectively, experimental findings indicate that the connection between oral health and cognition cannot be underestimated.”
This burgeoning corpus of scientific evidence carries substantial implications for our comprehension of human physiology and for the formulation of proactive public health strategies.
Satoshi Yamaguchi, the principal investigator of the Japanese study, commented on the implications of his team’s findings: “preserving a greater number of healthy teeth, free from periodontal disease, can potentially contribute to the safeguarding of brain health… Undertaking regular dental examinations is paramount for effectively managing the progression of periodontal disease.”
In essence, maintaining dental integrity extends beyond merely possessing a complete set of teeth; it necessitates the active prevention of periodontal disease to preclude adverse effects on cognitive function.
This is not merely an academic consideration. The World Health Organization estimates that severe periodontal disease, characterized by symptoms such as gingival bleeding and swelling, along with damage to the supportive structures of the teeth, affects approximately 19 percent of the global adult population.
Translating this into tangible figures, this suggests that upwards of one billion individuals may face an elevated risk of premature cognitive decline attributable to their oral health status.
Compounding the issue, the interplay between oral health and brain function appears to be bidirectional, implying that a decline in cognitive abilities can, in turn, precipitate less diligent oral hygiene practices.
Indeed, neurological conditions such as Alzheimer’s can impede the capacity for effective dental self-care. Individuals experiencing cognitive impairment may neglect oral hygiene routines or encounter difficulties complying with routine dental appointments, thereby initiating a detrimental cycle wherein cognitive deterioration leads to diminished dental standards, which subsequently exacerbates the underlying condition.
To effectively preempt this escalating predicament, policymakers and public health professionals must implement early interventions to address the root causes of the problem.
By championing the significance of daily brushing, flossing, consistent dental visits, and judicious dietary choices, these stakeholders can empower older adults to protect their oral cavities from the accumulation of plaque and pathogenic bacteria, thereby mitigating the risk of neurodegenerative diseases.
Furthermore, for those individuals already exhibiting early indications of dementia, familial support networks and caregivers can play a crucial role in establishing a resilient oral hygiene regimen customized to the specific needs of the patient.
Such tailored approaches might encompass digital reminders for brushing and flossing, or the provision of specialized oral care instruments like electric toothbrushes, which can offer enhanced ease of use. Certain dental practitioners also extend the convenience of home visits for dementia patients who face challenges in attending conventional appointments.
Encouraging patients to adopt supplementary preventative habits, such as the utilization of sugar-free chewing gum between meals, could also prove beneficial. Research indicates that the regular ingestion of sugar-free gum, in conjunction with brushing, can contribute to a reduction in the incidence of dental caries. Moreover, leaving packets of gum in visible locations for patients can serve as a passive prompt for chewing, diminishing the reliance on constant verbal reminders.
These modest yet persistent behavioral modifications can yield substantial long-term benefits, proving considerably more achievable to sustain than less frequent and more obtrusive dental interventions.
Given the considerable ramifications of compromised oral health on systemic well-being, including neurological function, it is imperative that dental care be elevated from a secondary concern to a priority. Proactive measures are fundamental to preserving the enduring vitality of the teeth and gums, and individuals with dementia should receive comprehensive support to facilitate adherence to these practices.
Undeniably, the battle against conditions such as Alzheimer’s cannot be solely attributed to oral health status. Multiple etiologies contribute to the emergence of dementia, and it would be imprudent to overemphasize the singular impact of oral cavity health on this complex pathological process.
Nevertheless, the extant evidence unequivocally demonstrates that interventions targeting oral health can contribute positively to the efforts to combat cognitive decline, and healthcare professionals bear a significant responsibility in disseminating this vital message.