When considering cardiovascular health through physical exertion, it is advisable to avoid reaching peak fitness too early in life. Emerging research indicates that to safeguard against elevated blood pressure in one’s later years, sustained engagement in exercise throughout middle age is essential.
However, a comprehensive investigation involving over 5,000 individuals across four American metropolitan areas has revealed that societal influences can pose greater obstacles to this endeavor for certain populations than for others.
“Adolescents and individuals in their early twenties often exhibit a high degree of physical vitality, but these patterns tend to shift as people age,” noted epidemiologist Kirsten Bibbins-Domingo from the University of California, San Francisco (UCSF) in April 2021, coinciding with the publication of the study.
While a substantial body of evidence supports the notion that physical activity contributes to lower blood pressure, the 2021 research underscores that “sustaining physical engagement during young adulthood—at levels exceeding prior recommendations—may be of particular significance,” Bibbins-Domingo commented.

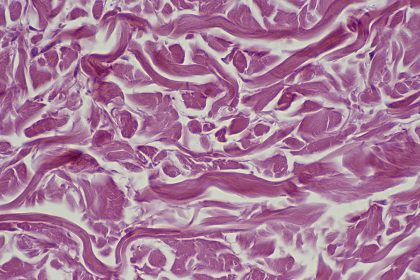
Hypertension, commonly recognized as high blood pressure, represents a critical health concern impacting a significant portion of the global population. Its sequelae can include myocardial infarction and cerebrovascular accidents, and it is also identified as a contributing factor to cognitive decline in later life.
According to data from the World Health Organization, more than a quarter of men and approximately one-fifth of women are affected by hypertension. A considerable number of individuals with elevated blood pressure remain unaware of their condition, earning it the moniker of the “silent killer.”
Nevertheless, avenues exist for mitigating high blood pressure; this particular research centers on the role of physical activity.
The study enrolled in excess of 5,100 adults whose health was monitored over a thirty-year period. This monitoring involved physical assessments alongside surveys pertaining to exercise habits, smoking status, and alcohol consumption.
At each scheduled clinical evaluation, blood pressure readings were taken on three separate occasions, with one-minute intervals between measurements. For the purpose of data analysis, participants were stratified into four distinct cohorts based on race and gender.
Consistently across all demographics—encompassing men, women, and both racial groups—a discernible decline in physical activity levels was observed between the ages of 18 and 40. Concurrently, hypertension incidence escalated, while physical activity diminished in subsequent decades.
“Close to half of our participants exhibited suboptimal levels of physical activity during young adulthood, which was significantly correlated with the emergence of hypertension. This finding suggests a need to elevate the baseline standard for physical activity,” stated lead author Jason Nagata, an expert in young adult medicine at UCSF.

Upon examining individuals who engaged in five hours of moderate exercise per week during their early adult years—thus surpassing the current minimum recommendation for adults by twofold—the researchers discovered a substantial reduction in hypertension risk. This benefit was particularly pronounced when individuals maintained these exercise regimens until the age of 60.
“Achieving at least double the current minimum adult guidelines for physical activity may offer superior benefits for hypertension prevention compared to merely adhering to the minimum recommendations,” the investigators articulated in their published paper.
However, augmenting weekly physical activity presents considerable challenges amidst significant life transitions and escalating responsibilities.
“This scenario may be particularly prevalent following high school, as opportunities for physical engagement lessen when young adults transition into higher education, the professional sphere, and parenthood, thereby diminishing available leisure time,” Nagata elaborated.
In another significant finding, the study illuminated the markedly different health trajectories experienced by Black men and women in comparison to their White counterparts. By the age of 40, physical activity levels stabilized among White men and women, whereas in Black participants, activity continued to decline.
By age 45, Black women exhibited higher rates of hypertension than White men, while White women in the study reported the lowest incidence of hypertension throughout their midlife.
By the age of 60, a substantial majority, ranging from 80 to 90 percent, of Black men and women had developed hypertension. This contrasts with just under 70 percent of White men and approximately half of White women.
The research team attributed these established racial disparities to a complex interplay of socioeconomic and environmental factors. While these specific determinants were not quantified within this study, the level of high school education was noted as a variable.
“Although Black male youth may demonstrate high participation in sports, various socioeconomic influences, the characteristics of their residential environments, and commitments related to work or family may impede sustained engagement in physical activity throughout adulthood,” Nagata commented.
The findings of this study were disseminated in the *American Journal of Preventive Medicine*.